Some of us keep it together so well, no one would ever guess we’re falling apart inside. IOP sounded like something “worse off” people needed—not people like us. But the truth is, burnout doesn’t always look messy. And high-functioning doesn’t mean thriving.
Here are five real stories from people who didn’t think they needed an intensive outpatient program—until something cracked, and they found relief in a place they never expected.
1. “I Was Still Showing Up to Work Every Day”
Paul, 42, had mastered the art of compartmentalizing. He was a respected project manager at a construction firm, juggling deadlines, team meetings, and client calls with a smile. What no one saw were the bottles hidden in his trunk. “I figured if I was still getting up, still producing, I must be fine,” he told me.
It wasn’t until his daughter found him unconscious in the garage, reeking of whiskey, that his reality snapped into focus. “I always said I didn’t need IOP because I wasn’t like the people you see on TV,” Paul said. “But that moment showed me I was closer to a breaking point than I realized.”
Midwest Recovery’s IOP gave him the structure to keep his job and the space to start healing. “I didn’t lose everything. But I came close. IOP helped me keep what matters.”
2. “I Thought I Could ‘Outsmart’ Addiction”
Jasmine was in the final stretch of her PhD in psychology. Her use of Adderall began as an academic edge, a few pills to help her power through exam season. But it didn’t stop there. “I thought if I knew enough, if I understood addiction, I could manage it myself.”
She didn’t want to be seen as someone who needed help. She had a therapist. She meditated. She excelled. But she was also crashing hard in secret.
“IOP wasn’t just for people in crisis,” she realized after attending an info session. “It was for people like me who were quietly falling apart under the weight of their own expectations.”
Through Midwest Recovery, Jasmine connected with other high-achieving individuals navigating the same contradictions. “I learned that being smart doesn’t mean being invulnerable. And that healing isn’t weakness.”
3. “I Was Afraid It Would Make Things Worse at Work”
Lamar worked in finance. His biggest fear wasn’t withdrawal or judgment—it was his boss finding out. “I thought if I got caught seeking treatment, my reputation would take a hit,” he shared. “IOP sounded too public. Too big.”
But when anxiety attacks started landing him in the ER, he knew something had to give. He found Midwest Recovery’s intensive outpatient program while scrolling on his lunch break. “They made it clear I could attend sessions around my work schedule. No overnight stays. No dramatic disappearances.”
He attended group in the evenings and still made his 9am meetings. “Eventually, I even opened up to my supervisor. He was more supportive than I expected. But I didn’t have to do that right away. IOP met me where I was.”
4. “I Didn’t Think I Deserved That Kind of Help”
Marta was the one everyone leaned on. A mother of two, church volunteer, and caregiver to her aging mom, she hid her drinking behind a curtain of competence. “I didn’t think I deserved something like IOP,” she said. “I wasn’t a mess. I was tired. That didn’t feel like enough of a reason.”
Her breakdown came in the Target parking lot. Crying uncontrollably after a cashier asked if she was okay. “That was it. That was my moment.”
IOP didn’t just give her tools to cut back—it gave her a place where she didn’t have to be the strong one for once. “They didn’t ask me to prove I was struggling enough. They just welcomed me.”
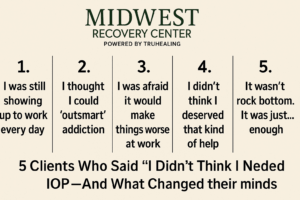
5. “It Wasn’t Rock Bottom. It Was Just… Enough”
Alex hadn’t lost their job or their apartment. They still made it to yoga class, still showed up to brunch. But inside, they felt flat. “I couldn’t feel joy anymore. I wasn’t panicking. I wasn’t crying. I was just… empty.”
They had assumed IOP was for people in crisis. But a friend shared their experience and something clicked. “They described the exact kind of numbness I was feeling. That’s when I realized I didn’t have to wait until things got worse.”
In IOP, Alex found language for what they were going through. “I didn’t need to spiral to deserve support. Feeling hollow was enough. Wanting more was enough.”
When You’re High-Functioning and Still Hurting
We don’t always break down in obvious ways. Sometimes the signs are subtle: a sense of emptiness, a short fuse, a reliance on substances to stay afloat. An intensive outpatient program like the one at Midwest Recovery Center in Toledo offers support that fits real life—jobs, families, and complicated inner worlds.
You don’t have to hit bottom. You just have to be ready for something different.
Frequently Asked Questions About Intensive Outpatient Programs (IOP)
What is an intensive outpatient program?
An IOP is a structured form of treatment that allows you to receive support several days a week while continuing to live at home and maintain work or school responsibilities. It typically includes group therapy, individual counseling, and psychoeducation.
How do I know if I need IOP?
If you’re struggling to manage substance use, stress, or emotional regulation on your own—but don’t need 24/7 supervision—IOP can be a powerful middle path. It’s designed for people who are functional, but not okay.
Can I attend IOP and still work?
Yes. Many IOPs, including Midwest Recovery’s program in Toledo, offer flexible scheduling, including evening and weekend sessions, to accommodate working adults.
Is IOP confidential?
Absolutely. Your privacy is protected by law. No one will know you’re attending unless you choose to tell them.
What makes IOP different from inpatient treatment?
Inpatient programs require you to live at the facility full-time. IOP lets you live at home and keep showing up for your life—while building the tools to show up differently.
📞 Ready to talk it through?
Call Midwest Recovery Center in Toledo at (833) 657-0858. You don’t have to prove how bad it is to get help. You just have to want better.
















